Compliance—
a Headway Guide
Navigating compliance can be time-consuming and stressful.
We’re committed to changing that.
Overview
Let's partner together to make compliance easy and stress-free.
Documentation, coding, and billing
Proper documentation and billing practices are a big part of compliance. Getting them right requires a level of detail that may not be immediately intuitive, but once you’ve got it down, the process becomes second nature. We’re going to get there together.
You have two options when keeping documentation:
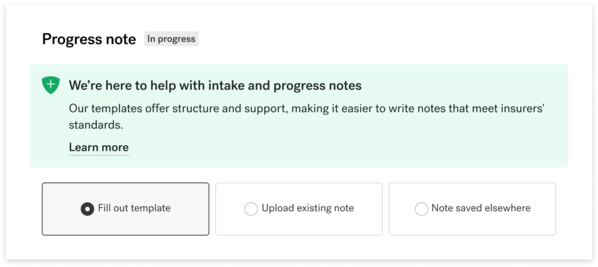
Headway templates
If you take your notes on Headway, the templates we provide are now optimized for compliance.
We’re taking the guesswork out of what you need to do and when you need to do it—and cutting down on the amount of note-taking required of you.
or
External notes
You can continue to take and store your notes using your preferred HIPAA-compliant method—on Headway, on a different EMR system, or offline.
In the event of a review or audit, you will be required to share your documentation with us. However, you are usually given the option to note that your documents are "saved elsewhere."
Periodic reviews
The possibility of an audit can be stressful, but it happens for good reasons.
Audits and routine reviews primarily exist to prevent fraud, waste, and abuse. More importantly, however, they protect clients by ensuring that providers are being held to the standards of clinical and service excellence that improve mental health symptoms, which matter to us all.
Don’t stress — this guide and our policies exist to help you avoid a disruptive audit.
How to be compliant
Compliance is largely about documentation and billing. Let’s talk through each.
Documentation
Our documentation requirements follow standards outlined by the American Medical Association (AMA), Centers for Medicare and Medicaid Services (CMS), National Committee for Quality Assurance (NCQA), commercial insurers, and other regulatory agencies.
Documentation of relevant aspects of client care, including documentation of medical necessity, should ideally be completed within 24 hours of visit, and no later than 72 hours.
While there’s a lot of information across those standards, we've broken down the key details below:
Types of documentation*
Initial assessment
An initial assessment (intake note) should be created when initiating a treatment relationship with a client.
Assessment should include:
- reason for seeking treatment
- past treatment history
- past successes or struggles
Resources
Headway template
See intake note example
Review policy
Treatment plan
A treatment plan establishes objectives and monitors progress. The plan includes a diagnosis and clearly establishes medical necessity for treatment.
Plans must be:
- created within 30 days of the start of treatment and updated bi-annually
- acknowledged by the client—via signature for in-person sessions or verbally for telehealth
Resources
See treatment plan example
Review policy
Progress notes
Progress notes should demonstrate a clear and comprehensive story of the client’s progress through treatment. Clear continuity of care is important — each note should lead into the next but also stand alone.
Progress notes should also refer back to the treatment plan and corresponding objectives.
Resources
Headway template
See progress note example
Review policy
* Use these recommendations as guidelines. To the extent your license or a particular insurer has stricter requirements than those set forth here, please follow those requirements.
Headway clinical templates
Headway's templates are optimized to keep you compliant while saving time. Learn more about our templates here:
Billing
Our goal is to assist you in submitting claims with CPT codes that are consistent with the services you provide and meet medical necessity requirements.
Pay attention to things like session length, location of service (e.g. face-to-face vs. telehealth) and types of therapy (e.g. individual vs. family). When in doubt, provide more documentation detail to help support the code you’ve submitted.
Commonly Asked Questions
We’re trusted with individuals’ most sensitive information and take protection very seriously. We’ve built a secure infrastructure and platform, maintain SOC 2* and HIPAA compliance, and follow industry best practices regarding cloud infrastructure and encryption.
*SOC 2 stands for Service Organization Control 2 and is a security framework that defines how companies should manage, process, and store customer data.
Headway limits requests, use, and disclosure of protected health information (PHI) to what is minimally necessary to accomplish the intended purpose of the appropriate request, use, or disclosure. An example of this is if a chart review is required for the purposes of processing insurance or ensuring compliance.
A dedicated, specialized team at Headway will review your charts on occasion, but only for the purposes of processing insurance, ensuring compliance, and performing other payment and healthcare operations functions. In addition, Headway team members receive specialized training on HIPAA, the importance of PHI safety, and the “minimum necessary” rule. Headway also proactively maintains an audit log of all access to client records.
If you have further questions or suspect any misuse, please contact us.
“Medical necessity” is a term that often includes a set of criteria that insurance companies use to determine whether or not they are going to pay for a billed service. If an insurance company deems a service “medically necessary” it means they agree that the service is clinically appropriate and needed based on diagnosis and documentation provided. However, a service meeting clinical criteria does not guarantee that the service will be covered. Other factors like coding (CPT), timeliness, and other applicable network rules may interfere with the success of the claim and reimbursement.
The 90837 CPT code is often understood to be the standard of a therapy session among providers. Generally speaking, it’s a code used to bill for an hour-long session of psychotherapy (i.e. talk therapy). However, insurers have a tendency to flag 90837 more frequently than other codes. This can result in payment delays, requests for clinical documentation to support the use of the 90837, and other confusion for what seems like a typical billing selection.
Providers use CPT (Current Procedural Terminology) codes when confirming sessions in our system. These codes correspond with things like the type of care provided (i.e., psychotherapy) and the length of time for the session.
E/M (Evaluation and Management) codes are a specific range of CPT codes used primarily by a certain kind of provider—typically physicians, psychiatrists, and nurse practitioners—who evaluate and manage a client’s health.

“Strong documentation and compliance are important ways we can advocate for our clients, ensuring that insurance companies understand clients' needs and recognize the exceptional care being delivered.”

Dr. Nicole Christian-Brathwaite, MD
Head of Medical and Clinical Strategy
Compliance reviews
Our job is to make working with insurance easy, including navigating reviews.
Why conduct reviews?
Reviews are conducted for the protection of our whole community — especially clients. Headway, as well as insurance companies, will periodically conduct reviews of claims and clinician records. This is done to ensure accuracy and compliance with regulatory standards, as well as address possible instances of fraud, waste, or abuse.
These reviews also give us the opportunity to help you improve your documentation and/or coding practices.
What happens during a review?
We understand that the thought of reviews and audits can be distressing. We’re on your side and are here to help navigate a complex system.
On occasion, Headway or an insurer will initiate a review. We will sometimes review charting documentation to look out for things like commonly missing items or repeated mistakes. Insurers might also request to review documentation to make sure it meets their requirements.
In either case, Headway’s job is to help assist you through the process with minimal inconvenience.
How we provide guidance
We’ll start by highlighting documentation details that might need updates, with clear context on which notes to modify and any relevant deadlines.
Personalized feedback
For one-off errors, missing information, and other quick fixes, we’ll provide personalized feedback to help you update your documentation to meet insurers’ standards. You may have the chance to supplement existing notes with an addendum.
Escalated education
If there are more serious issues or a pattern of repeated problems, Headway will work with you directly to identify the problems and address any concerns.
For more details on escalations, including situations involving fraud, waste, and abuse, please refer to our full Curative Action Policy.
Commonly Asked Questions
When your documentation is needed for a review, we’ll let you know right away. We’ll highlight relevant sessions in Sigmund, and — if applicable — highlight the items that likely need to be updated before submission.
This might mean we request that you upload an existing treatment plan or progress note on Headway. If your notes are already stored on Headway, we’ll flag any potential issues — such as a session length not properly matching the CPT code.
You’ll have a chance to review these queries, include any addenda as necessary, then submit your documentation. Check out this resource to see 10 of the items most commonly missing from chart documentation.
Using Headway’s in-product templates for initial assessments, treatment plans, and progress notes helps ensure you are meeting insurer standards and prepared for an audit. These templates are designed to cover the specific details insurers need to see, but are also streamlined to keep things as simple as possible.
If you’d prefer to store your notes outside of Headway, you can still quickly resolve any insurer review requests by being ready to provide this documentation to Headway within 3 days, should an insurer reach out to us.
Headway views clawbacks as a last resort. As your practice partner, our goal is to work collaboratively to resolve any concerns that arise. When we don’t receive communication from providers, we can’t properly communicate with insurers. In the event that a provider’s lack of communication makes it difficult to understand the services provided, we may have to return the payment to the insurer and we will adjust the provider's payments to reflect this. In the rare event that we have to adjust a provider's payment, we will communicate with the provider.
The great news is that these recoupment circumstances are avoidable.
In most cases, we will reach out to you directly if there’s a complication or question about the way something is submitted. We’ll do our best to avoid surprising you or editing your payments, and make an effort to work with you in advance if this comes up.

“As your practice partner, we’re here to help you develop consistent, compliant practices so we can navigate the complexities of the industry on your behalf.”

Innocent Turner, LCSW
Clinical Strategy Lead
Getting help
Headway is here to provide the support you need.
Find answers to common questions from providers
For additional questions about compliance or Headway in general, contact our support team.
Disclaimer
This document should be used for general informational purposes only. The contents do not constitute legal advice and should not be used as a substitute for advice from legal counsel.
Use this Clinical Documentation Policy and Procedure Manual as a reference guide, not as a definitive source of information regarding chart documentation requirements. We must work to ensure that all services submitted for reimbursement meet medical necessity and are based on accurate, complete, and timely documentation. It is the sole responsibility of every clinician to submit a complete accurate record of the services they provide and to document services in compliance with all applicable laws, best practices, and regulations.